After months of pain, multiple visits to your primary care doctor, sleepless nights, and inability to use an arm to put dishes away on the top shelf, your doctor finally gives you a diagnosis: frozen shoulder. The next thoughts are typical: “Is this a death sentence?”, “how do I unfreeze it?”, and “how could I have prevented this?”.
At this point, most people turn to Dr. Google to help them understand what is frozen shoulder (aka adhesive capsulitis), and more importantly, how to treat it. First, be careful what sites you get your information from. And, realize adhesive capsulitis is not a death sentence. You will survive and recover!
Let’s Synthesize What The Current Literature Says:
Frozen shoulder is a progressive loss of shoulder mobility with associated pain and disability. Pain typically develops slowly near the insertion of the deltoid (outside of your upper arm) and can radiate down the arm. We typically break adhesive capsulitis down into two stages: pain greater than stiffness or stiffness greater than pain. The former being the beginning stages and the latter being the later stages.
Generally, only 3-5% of the general population obtains a diagnosis of adhesive capsulitis. But, the incidence of having frozen shoulder increases to up to 30% if you have a diagnosis of diabetes. You are also at a slightly higher risk of developing it if you are female and between the ages of 40-60.
Frozen shoulder is further classified into primary idiopathic or secondary adhesive capsulitis. Primary idiopathic means there was no event leading to the start of the frozen shoulder. Secondary adhesive capsulitis is when a cause is known (i.e. issue with your rotator cuff, breast surgery, diabetes, hypothyroidism, etc.).
There is also a frozen shoulder that can develop from a traumatic fall, shoulder dislocation, and after shoulder surgery. These can come about due to prolonged use of a sling.
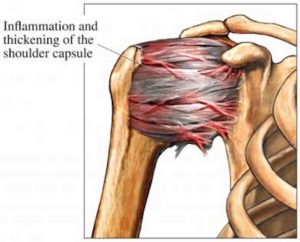
Image of the inflammation and thickening of the shoulder capsule for frozen shoulder
What’s The Prognosis Of A Frozen Shoulder?
Literature remains inconclusive. It was believed that shoulder range of motion and pain would dissipate after 2-3 years (with varying degrees of pain and motion during that time), but studies are starting to show a different story. We have been finding that adhesive capsulitis does not neatly progress through time in different stages like we had originally thought, and hoped.
What Should You Be On The Watch For?
Shoulder pain that starts with no mechanism of injury. Pain is typically on the outside of your arm but can go into your shoulder blade and down the arm. You will typically notice the pain before you start noticing any loss of range of motion. It amazes me that some don’t even notice that they have lost range of motion until they can’t lift their hand above their head! Pain is generally an ache that can become sharp with a fast motion. Most people start noticing sleep is very painful and limited. Also, washing your hair, completing personal hygiene, and putting on/taking off your shirt will become more difficult and painful.
So What Should You Do If You Think You May Have Or Are Developing A Frozen Shoulder?
Seek out a musculoskeletal expert who specializes in treating the shoulder!
There is hope for you to help alleviate the symptoms of a frozen shoulder and try to minimize the loss of function.
Want help diagnosing and treating a possible frozen shoulder?
Please fill out this form and we will schedule your evaluation to get you on the road to recovery!




